Top Links
Journal of Case Reports and Studies
ISSN: 2348-9820
Jugular Foramen Schwannoma Revealed By Unilateral Deafness
Copyright: © 2015 Benbakh M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Jugular foramen schwannomas arising from cranial nerves IX, X, and XI are uncommon pathological conditions, slowly growing benign tumors that constitute approximately 2.9 to 4% of all intracranial schwannomas [1,2]. Jugular foramen schwannomas represent 10-30% of all tumors observed around the jugular foramen [3,4]. The standard primary treatment for jugular foramen schwannomas is total surgical removal [5,6]. However, there is significant morbidity that results from extensive surgery and complex anatomical location. In the literature, there are a few published studies on radiosurgery for jugular foramen schwannomas [7-10]. The present study report a 28-year-old woman diagnosed with jugular foramen schwannomas who underwent gamma knife radiosurgery (GKS) in the IBN ROCHD university hospital of Casablanca, Morocco.
A 48-year-old woman presented with progressive right-sided hearing loss, chronic dysphonia and tinnitus. These signs were associated with chronic headache and dizziness for two years. On physical examination, the eardrums were normal. There was a right facial nerve dysfunction classified grade III according to House Brackmann grading system. Oral examination found a left side deviating uvula (curtain sign), tongue weakness with mild atrophy and abolition of gag reflex. Cervical examination showed a right shoulder weakness without palpable cervical mass. Laryngeal endoscopic exam found right vocal cord paralysis. There were no other significant cranial nerve findings. A finger-to-nose examination showed mild ataxia of the right upper limb. The gait was normal. An audiogram demonstrated a 60 dB sensorineural hearing loss. The stapedius reflex was absent. A CT scan was performed and found an enlargement of the jugular foramen and moderate enhancement with contrast medium (Figure 1). Magnetic resonance imaging (MRI) showed an isointense tumor on T1 weighted images (WI), hyperintense on T2 WI and enhance with gadolinium, this tumor extended to the internal auditory meatus (Figure 2). The patient was treated with GKS with a good clinical evolution.
The jugular foramen, located between the temporal bone laterally and the occipital bone medially, transmits the internal jugular vein, posterior meningeal artery, the IXth, Xth, and XIth cranial nerves and the inferior petrosal sinus.
A variety of neoplasms can arise within or around the jugular foramen. These include glomus tumors, the most common tumor, followed by schwannomas. In addition, meningiomas, chordomas, carcinomas, sarcomas, and neuroblastomas have been found in this area [11].
Jugular foramen schwannomas are rare, they commonly occur between the third and sixth decades of life, mainly in women [1,2,12-14]. The nerve of origin for the tumor is often identified only during surgery and the exact nerve of origin remains for most part unknown [15]. The most common symptom was hearing loss, followed by lower cranial nerve dysfunction. This was true in the present case report. The symptoms were very complete, so the decision was to perform radiological explorations (CT scan and MRI) without other hearing tests such auditory brainstem response (ABR) or otoacoustic emissions testing (OAE).
Jugular foramen schwannomas may originate from cisternal, foraminal, or extracranial portion of the nerves. Tumors originating from cisternal part grow more in the intracranial space and cerebellopontine angle; tumors originating from the foraminal portion predominantly expand the bone in the jugular foramen; and tumors originating from the extracranial part present with major extracranial growth [6,12,15-17]. For these tumors, many classifications have been developed, depending on their localization and radiologically extension [15,18]. Kaye's modified classification based on the findings from MRI is the most used [12]. Tumors that were primarily intracranial with only minor extension into bone were classified as type A; those that were located mainly within bone with or without an intracranial component were type B; those that were primarily extracranial with only minor extension into bone or the posterior fossa were type C. Type D (dumbbell-shaped) for tumors comprised lesions with significant intra- and extracranial portions.
CT scan orients the diagnosis by providing adequate data about the enlargement of the jugular canal and demonstrates either bone infiltration. MRI is only the tool to diagnose and to differentiate it from the other jugular foramen tumors. The imaging characteristics of jugular foramen schwannomas are usually iso- or hypointense on T1 WI and iso- or hyperintense on T2 WI and enhance with gadolinium [19].
Surgical resection is the standard procedure in patients with jugular foramen schwannomas [5,6]. However, there is significant morbidity that results from extensive surgery and complex anatomical location. There had been many approaches to this lesion: suboccipital, retrosigmoid, translabyrinthine, or infratemporal approach, but no general consensus has been reached. According to the literature, there are a few published studies on radiosurgery for jugular foramen schwannomas [7-10]. However, the tumor control rate for these tumors following GKS ranges between 96 and 100%, and the tumor shrinkage rate ranges between 47 and 52% [7,9,10,20]. This method is useful for residual tumors and also in the initial treatment of small tumors, especially when they are less than 3 cm and there is no lower cranial nerve palsy [20].
In this case report, the use of GKS for a jugular foramen schwannoma type C has a good outcome with no complication comparing to surgical resection.
Jugular foramen schwannoma are very rare tumors, and usually seen in adults. It can cause high intracranial pressure symptoms and cranial nerve abnormalities such as hearing loss, speech and swallowing disabilities .The surgery is challenging and associated with morbidity like cranial nerve palsy and cerebrospinal fluid (CSF) leak, radiation therapy or gamma knife can be preferred in uncomplicated small lesions. Surgery can be reserved for larger tumors.
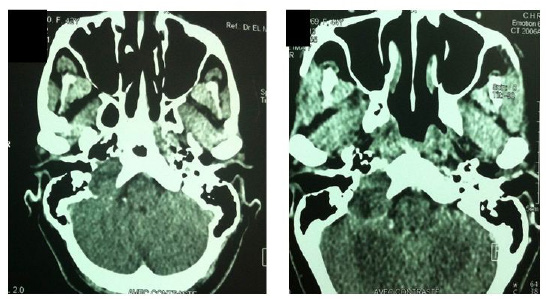 |
| Figure 1: Tumor swarming over the jugular, this mass became hyperdense after injection of contrast |
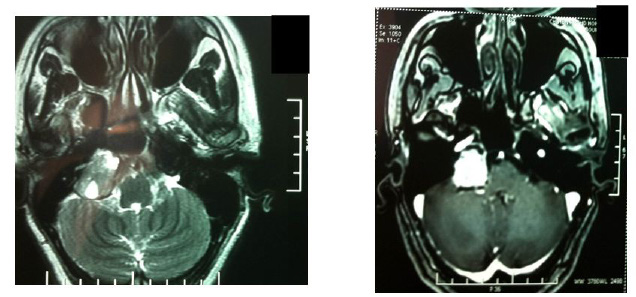 |
| Figure 2: MRI appearance of a schwannoma of mixed nerves |














